Uses of paracetamol
- Paracetamol is a widely used analgesic for:
- Headache
- Mild migraine
- Musculoskeletal pain
- Dysmenorrhoea (menstrual pain)
- Recommended as the first-choice analgesic in osteoarthritis
- Acts as an antipyretic and is prescribed for fevers of any cause
- Safe for use in children, with no risk of Reye’s syndrome
- Paracetamol has negligible anti-inflammatory actions
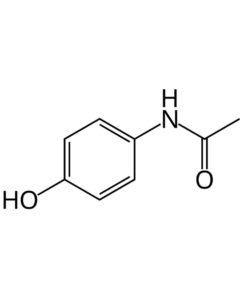
Class of Drug
- Analgesic drug
- Antipyretic drug
Mode of Administration and Dosage of paracetamol
- Available in tablet form (325 to 650 mg)
- Intravenous administration: 15 mg/kg
- Also available as a suppository
Mechanism of Action of paracetamol
- Paracetamol exhibits central analgesic action similar to that of aspirin
- It inhibits COX in the brain and is a poor inhibitor of prostaglandin synthesis in peripheral tissues
- Once absorbed, it raises the pain threshold, acting as a temporary analgesic
- Due to its inability to inhibit COX in the presence of peroxides (which are generated in sites of inflammation but not in the brain), paracetamol has poor anti-inflammatory effects. This explains its antipyretic and analgesic actions.
Metabolism of paracetamol
- Oral acetaminophen has excellent bioavailability
- Half-life of the drug is 2-3 hours
- Approximately one-fourth of the drug is protein-bound in plasma
- Peak plasma concentration occurs within 30 to 60 minutes after intake
- Metabolized through conjugation with glucuronic acid, sulfate, and cysteine
- 90-100% of the drug is excreted in urine within the first day after therapeutic dosage
- A small portion of acetaminophen undergoes CYP-mediated N-hydroxylation to form toxic NAPQI
Toxicity of paracetamol
- NAPQI, formed after CYP-mediated N-hydroxylation, is responsible for acetaminophen toxicity
- Hepatotoxicity is the primary concern with acetaminophen overdose, known as acute paracetamol poisoning
- Hepatotoxicity occurs in adults after ingesting 10 to 15 g (150–250 mg/kg)
- In children, a dose greater than 150 mg/kg is hepatotoxic
- A dose of 20-25 g can be potentially fatal
- Initial symptoms of hepatotoxicity may reflect gastric distress
- After 2-4 days, symptoms such as tender hepatomegaly, jaundice, coagulopathy, and renal impairment may develop
- After 72 hours, hepatic encephalopathy and liver enzyme abnormalities occur
- Severe liver damage and centrilobular necrosis are observed in patients
- Severe liver damage occurs in 90% of patients with plasma acetaminophen concentrations greater than 300 µg/mL at 4 hours or 45 µg/mL at 15 hours post-ingestion
- Activated charcoal, if administered within 4 hours of ingestion, can decrease acetaminophen absorption by 50-90%
- N-acetylcysteine (NAC) is the most accepted antidote for paracetamol overdose, as it detoxifies NAPQI
Adverse Effects of paracetamol
- Nausea
- Rashes
- Leukopenia (rare)
Contraindications of paracetamol
- Contraindicated in patients with existing liver and kidney diseases
- Contraindicated in premature infants weighing less than 2 kg due to the risk of hepatotoxicity
Additional Information
- Paracetamol, dose for dose, is equally effective to aspirin for non-inflammatory conditions and is much safer than aspirin in terms of gastric irritation, ulceration, and bleeding
- Patients contraindicated for aspirin may be prescribed paracetamol instead
- Some paracetamol combinations include:
- Paracetamol and Ibuprofen
- Paracetamol and Aceclofenac
- Paracetamol, Aspirin, and Caffeine
- Paracetamol and Tramadol